Today on Medscape
- Live Updates COVID-19
- Cardiology
- Diabetes & Endocrinology
- Family Medicine
- Hematology-Oncology
- Internal Medicine
- Neurology
- Psychiatry
Allergy & Immunology
Anesthesiology
Cardiology
Critical Care
Dermatology
Diabetes & Endocrinology
Emergency Medicine
Family Medicine
Gastroenterology
General Surgery
Hematology-Oncology
HIV/AIDS
Hospital Medicine
Infectious Diseases
Internal Medicine
Nephrology
Neurology
OB/GYN & Women's Health
Oncology
Ophthalmology
Orthopedics
Pathology & Lab Medicine
Pediatrics
Plastic Surgery
Psychiatry
Public Health
Pulmonary Medicine
Radiology
Rheumatology
Transplantation
Urology
Today on Medscape
Business of Medicine
Medical Lifestyle
Science & Technology
Medical Students
Nurses
Pharmacists
Residents
UK News & Perspectives View All
Featured News & Perspectives
Latest News View All
-
FDA Seeks More Information About RDEB Rx Under Review
-
 How to Improve Radiotherapy Decisions in Endometrial Cancer
How to Improve Radiotherapy Decisions in Endometrial Cancer -
 ACP-IM 2024Starting Points if Patient Chooses Medication Abortion
ACP-IM 2024Starting Points if Patient Chooses Medication Abortion -
 AAN 2024Largest CIDP Trial Offers Promising Results for Drug Combo
AAN 2024Largest CIDP Trial Offers Promising Results for Drug Combo -
 Planned Cesarean Delivery Doesn't Increase Infant Infections
Planned Cesarean Delivery Doesn't Increase Infant Infections -
 DUKPC 2024AI Model Predicts Inpatient Hypoglycemic Events
DUKPC 2024AI Model Predicts Inpatient Hypoglycemic Events -
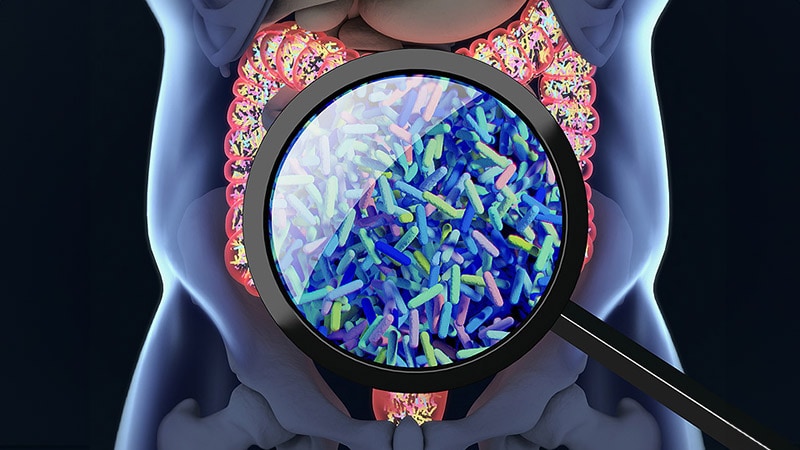
 Canada Will Likely Miss WHO's Hepatitis C Elimination Target
Canada Will Likely Miss WHO's Hepatitis C Elimination Target -
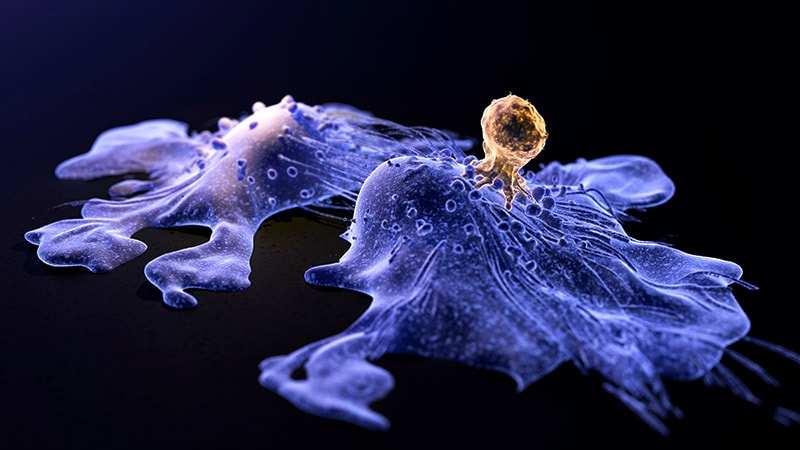 Timing Is Everything: CAR T for Follicular Lymphoma
Timing Is Everything: CAR T for Follicular Lymphoma




























.jpg)