Today on Medscape
- Live Updates COVID-19
- Cardiology
- Diabetes & Endocrinology
- Family Medicine
- Hematology-Oncology
- Internal Medicine
- Neurology
- Psychiatry
Allergy & Immunology
Anesthesiology
Cardiology
Critical Care
Dermatology
Diabetes & Endocrinology
Emergency Medicine
Family Medicine
Gastroenterology
General Surgery
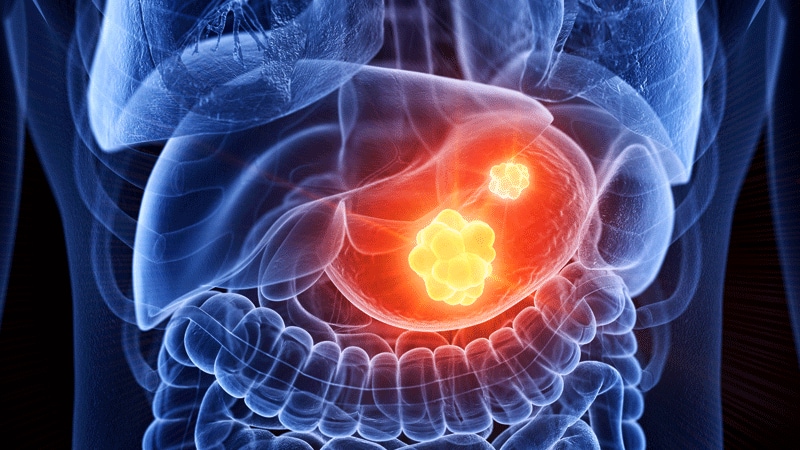
Hematology-Oncology
HIV/AIDS
Hospital Medicine
Infectious Diseases
Internal Medicine
Nephrology
Neurology
OB/GYN & Women's Health
Oncology
Ophthalmology
Orthopedics
Pathology & Lab Medicine
Pediatrics
Plastic Surgery
Psychiatry
Public Health
Pulmonary Medicine
Radiology
Rheumatology
Transplantation
Urology
Today on Medscape
Business of Medicine
Medical Lifestyle
Science & Technology
Medical Students
Nurses
Pharmacists
Residents
UK News & Perspectives View All
Featured News & Perspectives
Latest News View All
-
 ACP-IM 2024Hospice Handoffs May Lower Odds of Medicare Denials
ACP-IM 2024Hospice Handoffs May Lower Odds of Medicare Denials -
 EPA 2024Is Europe Taking Too Long to Adopt TMS for Major Depression?
EPA 2024Is Europe Taking Too Long to Adopt TMS for Major Depression? -
 AAN 2024ICI Tx in MS Patients With Comorbid Cancer: Reassuring Data
AAN 2024ICI Tx in MS Patients With Comorbid Cancer: Reassuring Data -
 ACP-IM 2024Menopause, RSV, and More: 4 New Meds to Know
ACP-IM 2024Menopause, RSV, and More: 4 New Meds to Know -
 New Screening Protocol May Improve Prostate Cancer Detection
New Screening Protocol May Improve Prostate Cancer Detection -
ASLMS 2024Less PIH After Modified Laser Rx for Lentigines Reported
-
 AAN 2024Lidocaine Nerve Block Effective for Severe Migraine in Kids
AAN 2024Lidocaine Nerve Block Effective for Severe Migraine in Kids -
 Does TIPP Reduce Childhood Injuries?
Does TIPP Reduce Childhood Injuries?





























.jpg)